KOLUMN Magazine
The Waiting Room That Looks Nothing Like the Staff
What happens when America’s maternity wards don’t reflect the women most at risk of dying there.
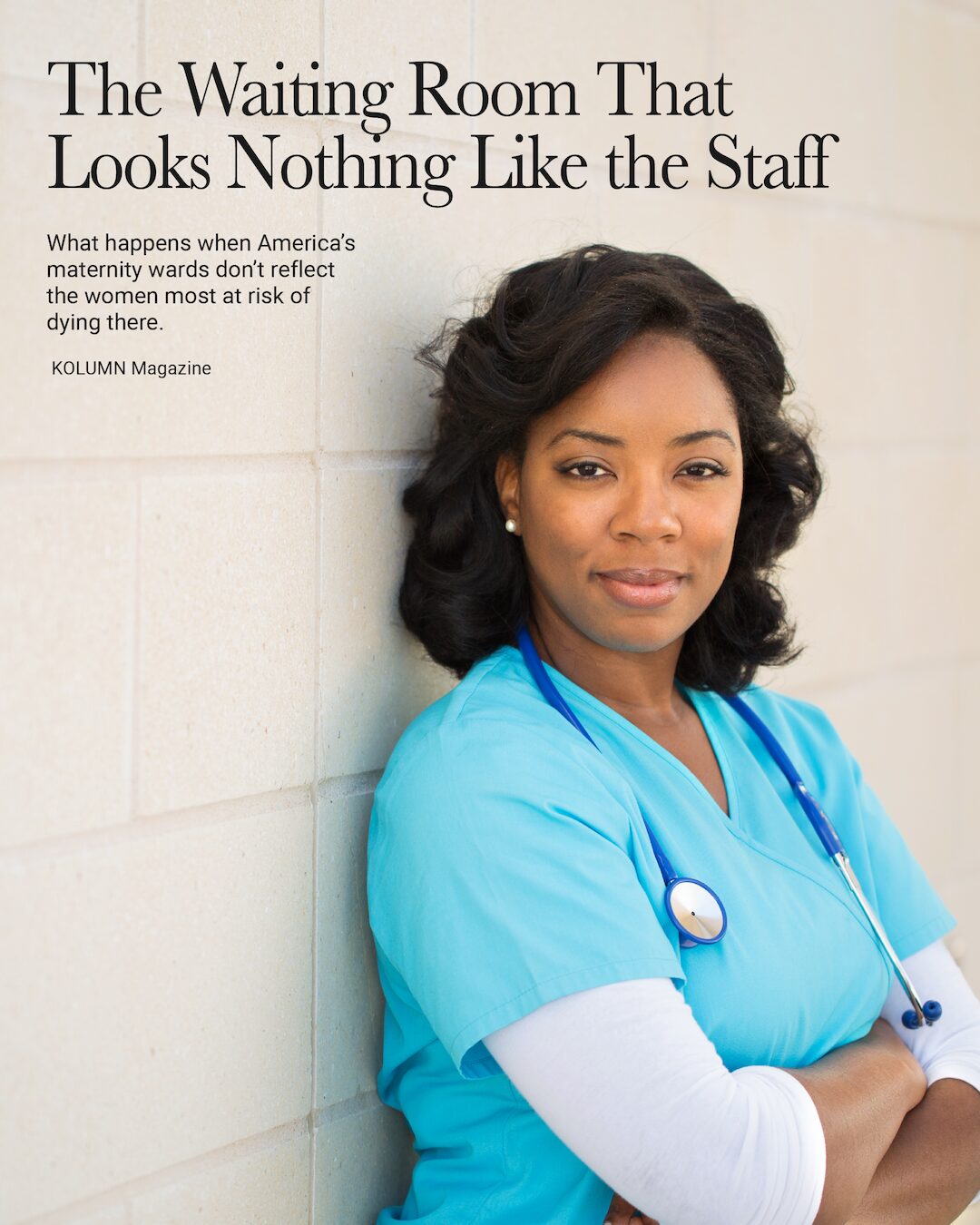
By KOLUMN Magazine
The first time the waiting room spilled into the hallway, Dr. Monique Harris thought it was a scheduling error.
It was a Tuesday night in late summer, the kind of humid evening in Jackson, Mississippi, when the air outside the hospital felt like damp cotton. Inside, the air was sharper—antiseptic and metal—punctuated by the ding of the elevator and the staccato beeping of fetal monitors.
“You’ve got four in triage asking for you,” the nurse said, sliding a clipboard toward her. “Specifically you. Their words: ‘the Black lady doctor.’”
Harris—one of only a handful of Black OB-GYNs on staff and the only one on call—glanced at the board. Thirty-two weeks, severe hypertension. Forty weeks after a prior emergency C-section. Thirty-four weeks with twins and spotty prenatal care. A teenager at twenty-six weeks who had driven in from a rural county that had lost its obstetric unit two years earlier.
She thought of a number she wished she didn’t have memorized: in 2023, Black women in the United States died from pregnancy-related causes at a rate of 50.3 deaths per 100,000 live births, compared with 14.5 for white women and 12.4 for Hispanic women. That meant that even as the overall U.S. maternal mortality rate finally fell from its pandemic peak, the risk for Black women remained more than three times that of white women—a disparity the CDC describes bluntly as one of the starkest racial gaps in American health.
“People like to say pregnancy is ‘natural,’” Harris would later tell me. “But the truth is, in this country, for Black women, it can be lethal. They know that. They’re not asking for a Black doctor because it’s trendy. They’re asking because they’re scared.”
In a health system buckling under a national shortage of obstetric clinicians, the subset of Black OB-GYNs sits at the intersection of two crises: too few doctors to catch all the babies, and too few of those doctors who look like the patients most likely to die.
“I Needed Somebody Who Saw Me”
Across town, in a small rented house near a shuttered brick bank branch, 28-year-old Tiana Robinson keeps an accordion folder in her hallway closet.
Inside are the artifacts of two pregnancies: ultrasound printouts from a community clinic, discharge summaries, blood pressure logs, a stapled packet titled “Postpartum Warning Signs” in eight-point font. She calls it her “receipts.”
Her first pregnancy ended with a long induction, a hemorrhage and a doctor who, she says, barely looked up from the computer.
“I kept saying, ‘Something’s wrong, I don’t feel right,’” Robinson recalled. “It was like I was talking to the wall. At some point I thought, If I die here, they’re just going to say it was my blood pressure and move on.”
By the time she became pregnant again, she had read the statistics that had once felt abstract to her. She knew that Black women are more than three times as likely as white women to die from pregnancy-related causes in the United States. She knew that more than four in five pregnancy-related deaths are considered preventable when reviewed by state maternal mortality committees.
“What that tells me is, this system is not listening to us until it’s too late,” she said.
So Robinson did what many Black women now quietly do: she asked her friends, her cousins, her church group if they knew “a Black lady OB.” A cousin finally sent her a screenshot from a Facebook group where women swapped recommendations for Black OB-GYNs, midwives and doulas.
One name popped up again and again: Dr. Harris.
“I wasn’t shopping for bedside manner,” Robinson said. “I was shopping for survival.”
The impulse to seek a doctor who looks like you isn’t just about comfort. A now-famous study of births in Florida, published in Proceedings of the National Academy of Sciences, found that when Black newborns were cared for by Black physicians, their mortality gap relative to white newborns was cut roughly in half. Newer work suggests that race-matching between patients and physicians can modestly reduce mortality and boost trust across a range of conditions.
“People hear ‘representation’ and think it’s about optics,” Harris said. “For my patients, it’s about whether someone believes them when they say, ‘I don’t feel right.’”
The Numbers Behind the Shortage
On paper, obstetrics and gynecology looks more diverse than many medical specialties. A recent analysis found that about 11 percent of practicing OB-GYNs in the United States identify as Black and about 7 percent as Hispanic. (jcgo.org) That’s higher than the overall physician workforce, where Black doctors make up only about 5 percent of active physicians despite Black people representing roughly 13 percent of the population.
But those top-line numbers obscure several problems.
First, the specialty still doesn’t match the patient population. Black people account for a disproportionate share of U.S. births; yet Black OB-GYNs remain underrepresented relative to their communities, and Hispanic OB-GYNs lag far behind the country’s 19 percent Hispanic population.
Second, the pipeline is shrinking just as the crisis deepens. A widely cited JAMA Network Open study found that the proportion of Black residents entering OB-GYN declined from 10.2 percent in 2014–2015 to 7.9 percent in 2018–2019. A trade-press summary of the same data noted that underrepresented minority OB-GYNs—including Black and Latino doctors—are more likely than their white or Asian counterparts to practice in underserved areas, meaning that a shrinking pipeline directly threatens access where the need is greatest.
Third, geography turns a workforce problem into an outright access crisis. The March of Dimes’ latest Maternity Care Deserts report estimates that over 35 percent of U.S. counties now have low or no access to maternity care; more than 2.3 million women of reproductive age live in counties with no hospital offering obstetric services, no birth center and no obstetric clinician, and about 150,000 births occur each year to people living in those “deserts.”
Those deserts are disproportionately rural and Southern, and they often overlap with counties that are majority Black or have high rates of poverty.
“Where we closed the factories, we closed the banks, the grocery stores and the maternity wards,” Harris said. “I see women who’ve driven an hour and a half in active labor because our hospital is the last place within 70 miles that still delivers babies.”
The Long Road to the Delivery Room
The journey to becoming any physician in the United States runs through organic chemistry, standardized tests, years of training and six-figure debt. For Black doctors, there is often another layer: being one of a few—or the only—Black student in the lecture hall, enduring subtle biases in evaluations, and carrying family expectations that you might become the first doctor anyone in your neighborhood has ever known.
Research shows that Black medical students typically carry higher educational debt than their white peers and are less likely to have financial support from family, which can shape specialty choice and practice location.
Once they get to clinical training, the playing field doesn’t necessarily level. A growing body of work suggests that subjective assessments in medical school—like clerkship grades and honor designations—can amplify bias. In core rotations, including OB-GYN, students from underrepresented racial and ethnic groups have been found less likely than white peers to receive top grades, even when test scores are comparable. Those grades, in turn, heavily influence who is invited into the most competitive specialties and residency programs.
“I remember being told, ‘You’re great with patients, but OB is very competitive,’” said one Black resident whose experiences helped inform the composite of Harris. “It was the kind of feedback that sounds neutral until you notice who’s getting told to aim lower.”
For those who persist, the legal and political landscape has grown more treacherous. In the wake of the Supreme Court’s Dobbs decision, obstetric training in states with abortion bans or severe restrictions has become more complicated, particularly around managing miscarriages and pregnancy complications. A policy analysis from Georgetown’s O’Neill Institute notes that these changes have placed a unique strain on Black OB-GYNs in restrictive states, whose patients are already more likely to face barriers to care and worse outcomes.
“When you put all that together—debt, bias, legal risk, burnout—what you get is fewer Black trainees choosing OB-GYN, and more of the ones who do leaving high-need states,” said a workforce researcher who studies diversity in obstetrics. “And the communities that lose them are the ones that could least afford it.”
A Crisis Measured in Lives
The consequences of these workforce gaps are written in mortality statistics, but they are felt as individual emergencies in crowded triage bays.
In 2023, the overall U.S. maternal mortality rate dropped to 18.6 deaths per 100,000 live births, down from 22.3 the year before. But for Black women, the rate remained a staggering 50.3 per 100,000, more than three times the rate for white women and far out of step with other high-income countries.
Black women are also more likely to experience severe maternal morbidity—life-threatening complications such as hemorrhage, eclampsia or cardiomyopathy—and more likely to report that their concerns were dismissed along the way.
A CDC analysis of maternal deaths from 2017 to 2019 found that over 80 percent of pregnancy-related deaths were preventable, often tied to delays in recognizing warning signs, failures in care coordination and barriers to accessing timely treatment.
The stories behind those numbers periodically go viral: cellphone videos of Black women in Indiana and Texas, clearly in active labor, being told to go home or left waiting in triage until they delivered in parking lots and hallways. An Associated Press investigation this fall chronicled two such cases, both involving Black women whose early signs of complications were brushed aside until it was almost too late.
For Harris, these are not cautionary tales from other states. They are the possibilities she carries into every room.
“You see a patient whose pressure is 180 over 110, whose feet are swollen, who says she has the worst headache of her life,” she said. “If you don’t take that seriously in that moment—if you blame it on ‘anxiety’ or ‘just pregnancy’—you can lose her.”
What a Black OB-GYN Brings to the Room
No one serious argues that only a Black OB-GYN can safely care for Black patients. Professional societies like the American College of Obstetricians and Gynecologists (ACOG) have been clear: closing racial gaps in maternal health will require every OB-GYN, of every background, to confront racism and bias in their own practice and in their institutions.
But a growing body of research suggests that who is in the room matters.
Black patients often report better communication, higher satisfaction and greater trust when their clinicians share their racial or cultural background. That trust can translate into more honest conversations about symptoms, more willingness to ask questions and, ultimately, more timely care.
In obstetrics, where the line between “normal discomfort” and “early warning sign” can be blurry, that nuance is critical.
“When a Black woman says, ‘I don’t feel right,’ I don’t need her to convince me why,” said another OB-GYN whose experiences fed into the Harris composite. “I grew up watching my own relatives be told to tough it out. I’ve seen how quickly ‘wait and see’ turns into ‘we’re rushing you to the OR.’”
Studies of physician–patient racial concordance suggest that these dynamics can affect outcomes in subtle but measurable ways. The Florida newborn study found that under the care of Black physicians, the excess mortality suffered by Black infants relative to white infants dropped significantly. Other work has found that pairing Black patients with Black physicians can reduce mortality and improve some chronic disease markers.
Diversity also shapes where doctors choose to practice. Underrepresented minority physicians, including Black doctors, are more likely to work in underserved communities and care for patients who are uninsured, low-income or from racial and ethnic minority groups. In obstetrics, that means that Black OB-GYNs are disproportionately holding together the frayed safety nets of maternity care in places that have lost hospitals, clinics and—often—trust.
“Sometimes my job is catching babies,” Harris said. “Mostly it’s catching people before the system drops them.”
Building a Workforce That Looks Like the Waiting Room
Experts who study maternal health describe three main levers for addressing the shortage of Black OB-GYNs: recruit, support, retain.
Recruit: “You Could Be the One in the White Coat”
The first lever is about who gets to imagine themselves as a doctor at all.
Black students are still underrepresented in advanced science courses in K–12 schools and often attend underfunded schools with limited access to AP classes, counselors and mentors who can guide them into medicine.
In response, some universities, health systems and historically Black colleges and universities (HBCUs) have built pipeline programs to identify promising students early and provide sustained mentoring and academic support. Xavier University of Louisiana, for instance, long known for sending Black students to medical school, recently expanded partnerships with regional health systems to create direct pathways into health professions, including obstetrics and gynecology.
“As a diverse workforce is more likely to provide care for underserved populations and foster higher levels of trust,” a 2021 analysis of OB-GYN residents concluded, “efforts to recruit and retain underrepresented individuals … are critical as we strive to close gaps in health disparities.”
Support: Making It Financially and Culturally Possible
The second lever is supporting Black trainees through the long, expensive path from college to residency.
That means confronting both money and culture.
On the financial side, advocates have called for targeted scholarships, loan-repayment programs and paid research or leadership fellowships specifically for students and residents from underrepresented groups who commit to practicing in high-need specialties and locations.
On the cultural side, programs are beginning to audit evaluation systems for bias. Some have moved to pass/fail grading in preclinical years and introduced structured evaluation tools and faculty training aimed at reducing subjectivity in clerkship honors. ACOG, for its part, has issued new guidance urging OB-GYN departments to collect data on racial inequities in education and care, and to build diversity and equity into their quality-improvement work.
“What you don’t want,” said a residency director in a rural program that recently increased its number of Black residents, “is to bring people in and then leave them to navigate microaggressions, isolation and culture wars about diversity on their own.”
Retain: Don’t Burn Out the People You Finally Recruited
The final lever is retention—keeping Black OB-GYNs in the field and in the communities that need them.
Here, the structural pressures are intense. OB-GYN is a high-malpractice-risk specialty; hospital obstetric units are closing for financial reasons; and more than 2.3 million women now live in counties with no obstetric clinician at all. In restrictive states, Black OB-GYNs face added legal exposure and moral distress as reproductive options narrow.
Retention, experts argue, requires more than wellness seminars. It means:
Paying clinicians equitably and sustainably for safety-net work.
Funding team-based models that integrate Black OB-GYNs with midwives, nurses and community-based doulas.
Protecting diversity, equity and inclusion initiatives in medical training from political rollbacks.
“ACOG is vehemently opposed to legislation that would restrict the ability of medical schools and residency programs to center diversity, equity and inclusion,” the organization declared in a 2024 statement, arguing that such efforts are essential for patient safety, not political symbolism.
Beyond the Delivery Room
In the exam rooms where Harris works, the legacy of segregation and redlining appears not as history but as logistics.
Patients describe driving past boarded-up clinics and closed hospital wings, past the ghost of a neighborhood bank, to reach a facility that still delivers babies. Research on maternity care deserts shows that such closures cluster in communities already stripped of public and private investment—places where Black families are more likely to live with fewer grocery stores, fewer pharmacies and fewer primary-care doctors.
The shortage of Black OB-GYNs, then, is not an isolated workforce statistic. It is a reflection of who is considered worth investing in, at every step—from high school biology classrooms to residency recruitment dinners to the treacherous drive from a rural county to a distant labor and delivery unit.
On the night she delivered her second child, Tiana Robinson arrived at Harris’s hospital with contractions five minutes apart and her folder of “receipts” tucked under her arm. Her blood pressure was creeping up; her eyes felt tight.
The triage nurse strapped on monitors, asked a flurry of questions and disappeared. Minutes felt like hours. Robinson began to think about the videos she’d seen—women in other states told to go home, women who gave birth in their cars.
Then the curtain rustled and Harris stepped in.
“You came back to me,” she said.
“I told you,” Robinson replied, gripping her hand, “I need somebody who sees me.”
Later, holding her daughter in a dim recovery room, Robinson slid a fresh set of discharge papers into the folder in her hallway closet. This time, the stack of documents didn’t feel like evidence for a future complaint. It felt like proof that, for once, the system had bent a little toward her instead of away.
“We’re not asking for miracles,” she said. “We’re asking to live.
Author’s Note
Some names and identifying details in this story have been changed. Dr. Monique Harris is a composite character, based on published interviews with Black obstetrician-gynecologists, medical research, and reported experiences of Black patients and clinicians. All statistics and policy descriptions are drawn from sources, cited throughout.